Breast Thermography
Infrared Breast Thermography is another assessment tool we offer for our Greenville, Spartanburg, and Anderson area patients. It is a safe, non-ionizing, non-contact study of breast skin temperature that is useful as a breast thermal findings assessment. It is useful as in the detection of physiologic changes such as hypervascularity, hyperthermia, hormonal imbalance, lymphatic edema, ductal congestion, chest wall and other thoracic pain syndromes. Internationally peer reviewed Guidelines for Breast Thermography have been developed by the American Academy of Thermology in 2012 and are restated every three years. These guidelines support breast thermal imaging as a breast thermal findings assessment, the results of which can be used to assist in clinical decision making regarding breast health, not unlike high blood pressure screening for vascular disease.
Thermography measures, images and maps microcirculatory shunting associated with breast circulatory changes in the skin. Hepatic congestion, musculoskeletal conditions, sex hormones such as estrogen and progesterone, can affect breast physiology and circulation. Serial studies can also be helpful in monitoring the effects of hormone replacement therapy or the treatment of fibrocystic disease.
While breast thermography can play a useful role in monitoring treatment effects, as with most physiologic studies the results of anatomic testing (such as mammography or MRI) may not correlate or may not even be present despite the presence of physiologic change (physiologic findings tend to predate structural findings). Thermography can however play an important adjunctive role in clinical diagnosis and in distinguishing between benign, early, advanced, and progressive disease. The role of Thermography in cancer detection is frequently misunderstood and deserves special attention.
The concept of using breast thermography to evaluate for angiogenesis is one reason breast thermography used to be called a breast risk health assessment. The idea is that as cancer cells need increased blood flow in order to “take” over surrounding breast tissue, progressive hypervascularity on a breast thermography is an harbinger of angiogenesis. Since cancer cells also have an increased metabolic rate, physiologic changes associated with that can be seen as hyperthermia with infrared imaging. If superficial enough, hyperthermia can be seen with infrared imaging to more readily detect and map out increases in temperature compared to surrounding normal tissue. By studying breast tissue with infrared imaging early changes in blood flow can be detected and progressive changes can be assessed over time.
And there is literature to support this contention. For example, in 1997 Gamagami, Silverstein & Waisman published:
- Angiogenesis was the first sign appearing on mammography before the appearance of image of breast cancer, predicting in 91 % of the cases which breast might develop breast carcinoma. This is an important finding in the detection of the early stages of breast cancer development.
- Infrared imaging goes hand in hand with mammography. Hypervascularity and hyperthermia could be shown in 86% of non-palpable breast cancer. In 15% it helped to detect the cancer upon an unsuspicious image on mammography.
- Infrared imaging was found to be the only test showing the efficiency of chemotherapy in inflammatory breast carcinoma.
While Breast Thermography is not a stand alone tool in the diagnosis of breast disease no screening tool (including X-ray mammography and Ultrasound) provides excellent predictability when used by itself. A combination of tools, including those that incorporate Infrared Thermography, have been shown to boost both sensitivity and specificity compared to using a single study method.
Authors of a 4-year, five-institution study published in the American Journal of Radiology (2003) concluded that Infrared Mammography is a safe noninvasive procedure that is valuable as an adjunct to X-Ray Mammography in determining whether a lesion is benign or malignant. While acceptance of findings remains controversial this study reported that there was 97% sensitivity when identified lesions were biopsied, however only a 14% specificity. This means that Infrared Mammography is very sensitive at detection, however identified lesions are most often not cancer (usually they are microcalcifications). There was also a 95% negative predictive value, and a 24% positive predictive value. It has been argued that this means if an breast thermal findings are minimal or absent then there is a 95% chance that there is no cancer and that if they are positive than there is a 24% chance that cancer may later be discovered.
In 2008 The American Journal of Surgery (pages 523-526) published that Infrared Mammography identified 58 of 60 malignancies, with 97% sensitivity, 44% specificity, and 82% negative predictive value. The authors concluded that Infrared Mammography is a valuable adjunct to X-ray mammography and ultrasound, especially in women with dense breast tissue. Other indications include small breasts, post implant breasts, post mastectomy breasts, those looking for additional information, and to follow the effects of treatment.
To this day, the role of breast thermography in cancer detection is still debated. Fortunately, for medical practitioners who believe that a breast thermal findings assessment is a valuable tool that can help with clinical decision making, The American Academy of Thermology has published Internationally peer reviewed Guidelines that provide a blueprint for its proper use and application.
In summary, thermal imaging is an examination of physiology that is complimentary to anatomical imaging techniques. Although proven to be highly sensitive, thermal imaging is an adjunctive procedure; and as such, it is not intended to replace anatomic studies such as mammography, ultrasound, MRI, CT, X-ray, or others.
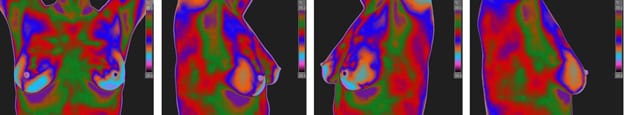
Example Breast Thermography Protocol Images:

Dr. Schwartz is President of the American Academy of Thermology





